Data Migration in Healthcare: Safeguarding PHI While Modernizing Clinical Systems
If there’s one thing everyone in healthcare IT quietly agrees on, it’s this: modernizing clinical systems sounds exciting until you reach the data migration stage. That’s where the optimism slows down.
Healthcare carries some of the most sensitive, messy, interconnected, and historically layered data of any industry. And before any organization can proudly announce a new EHR, a cloud transformation, a revamped lab system, or a consolidated clinical platform, the data has to move — safely, accurately, and in a way that respects the legal and ethical weight of Protected Health Information (PHI).
PHI isn’t just another dataset. It’s the living history of patients — what they’ve been diagnosed with, the medications they rely on, how they responded to treatments, and the nuances that clinicians depend on every single day. Mishandle it, and the consequences can reach far beyond IT; this is the kind of data that can alter a clinical decision or put a physician in a difficult situation. So the question isn’t whether data migration is essential; it’s how to do it responsibly.
This editorial-style deep dive explores the realities of PHI migration, explains why healthcare data is uniquely challenging, and lays out a practical, compliant framework for moving from legacy systems to modern platforms — all supported by ChainSys Smart Data Platform tools that have been used in real enterprise transformations.
A lot has changed in the last decade. Healthcare systems, once built around isolated applications, now need real-time communication with everything from HIEs to national registries to patient-facing apps. And with interoperability moving toward FHIR APIs, organizations can’t sit comfortably on platforms built 20 years ago.
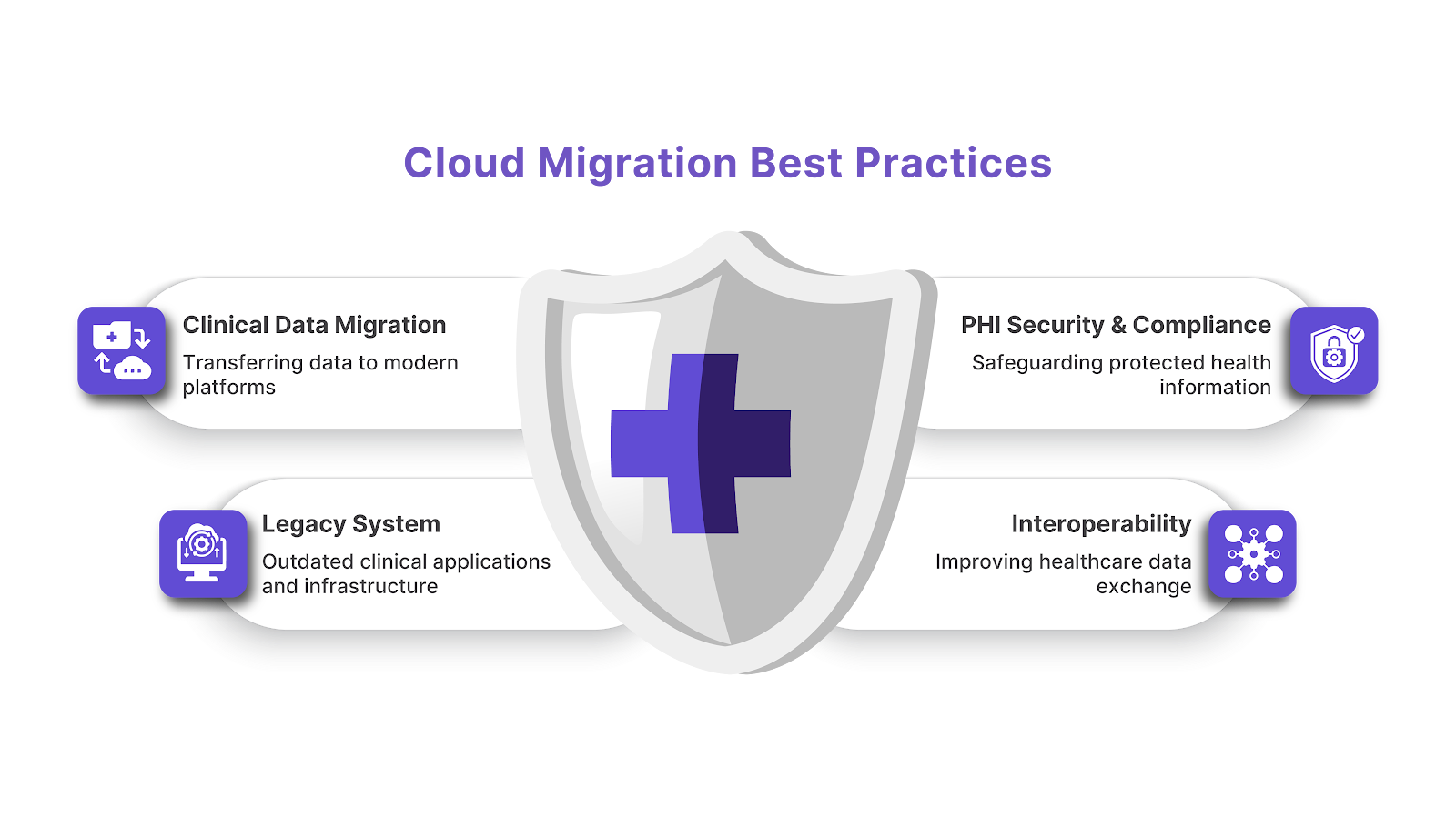
These days, exchanging clean, structured data isn’t optional. Governments are pushing interoperability. Payers expect it. Patients expect access on demand. Legacy systems struggle with this because they rely on outdated HL7 interfaces that were never designed for the world we live in now.
Most healthcare CIOs are steering their organizations toward cloud ecosystems — Oracle Cloud, AWS, Azure — not because it’s trendy, but because a modern hospital simply can’t keep pace using old infrastructure. Cloud security, resilience, and scalability just make sense. To get there? Data has to be extracted, cleaned, transformed, and reloaded.
Healthcare is the most targeted sector for ransomware. Attackers don’t want your office calendar or HR directory; they want clinical data. Many older systems simply can’t keep up with today’s cybersecurity expectations, making modernization inevitable.
Imaging files are larger, clinical notes are longer, and the variety of digital tools used in care is far beyond what older systems were built for. Healthcare is generating more data in a month than it used to generate in entire years. Migration becomes the highway that moves all of this to a future-ready environment.
Healthcare leaders increasingly want prediction, pattern recognition, and intelligent support. Those tools only work with clean, structured data — which is precisely what a good migration prepares for.
The very term “PHI” tends to make healthcare teams more alert, and for good reason. PHI isn’t just personal — HIPAA protects it, it’s under constant scrutiny during audits, and it holds emotional weight for patients and their families
Unlike some industries where data can be neatly consolidated, healthcare is messy. A single patient’s information can be spread across EHRs, lab systems, radiology archives, pharmacy systems, billing platforms, and portals. A migration must pull all of this together without altering meaning.
If billing is wrong, that’s an inconvenience. If a patient’s allergy is wrong, that’s a risk. Clinical integrity matters, and mistakes made during migration can easily ripple into care delivery.
Hospitals cannot “pause” operations, not even for a weekend. Data is constantly changing — new labs, edited notes, pharmacy updates, new admissions. The migration strategy must keep pace without sacrificing accuracy.
Fragmented Systems Every hospital runs a mix of old and new tools. Some still rely on homegrown systems built by a retired developer in 2008. Others have niche departmental applications. Migrating this patchwork requires careful choreography.
Multiple Coding Standards ICD-10, SNOMED CT, LOINC, NDC, CPT, HCPCS — healthcare has a language of its own. Mapping these cleanly into a modern system is a clinical exercise as much as a technical one.
A Mix of Structured and Unstructured Data Clinical notes, HL7 feeds, PDF discharge summaries, scanned referrals, pathology reports, and imaging metadata — all must be maintained and migrated in usable form.
Unforgiving Downtime Constraints A finance system can tolerate a weekend outage. An ICU cannot. That’s why NZDT (near-zero downtime) migration strategies aren’t optional; they’re foundational.
A Realistic, HIPAA-Aligned Framework for Secure Healthcare Data Migration Below is a detailed migration approach written in a way that mirrors how healthcare teams actually operate — grounded, realistic, and aligned with real-world governance practices.
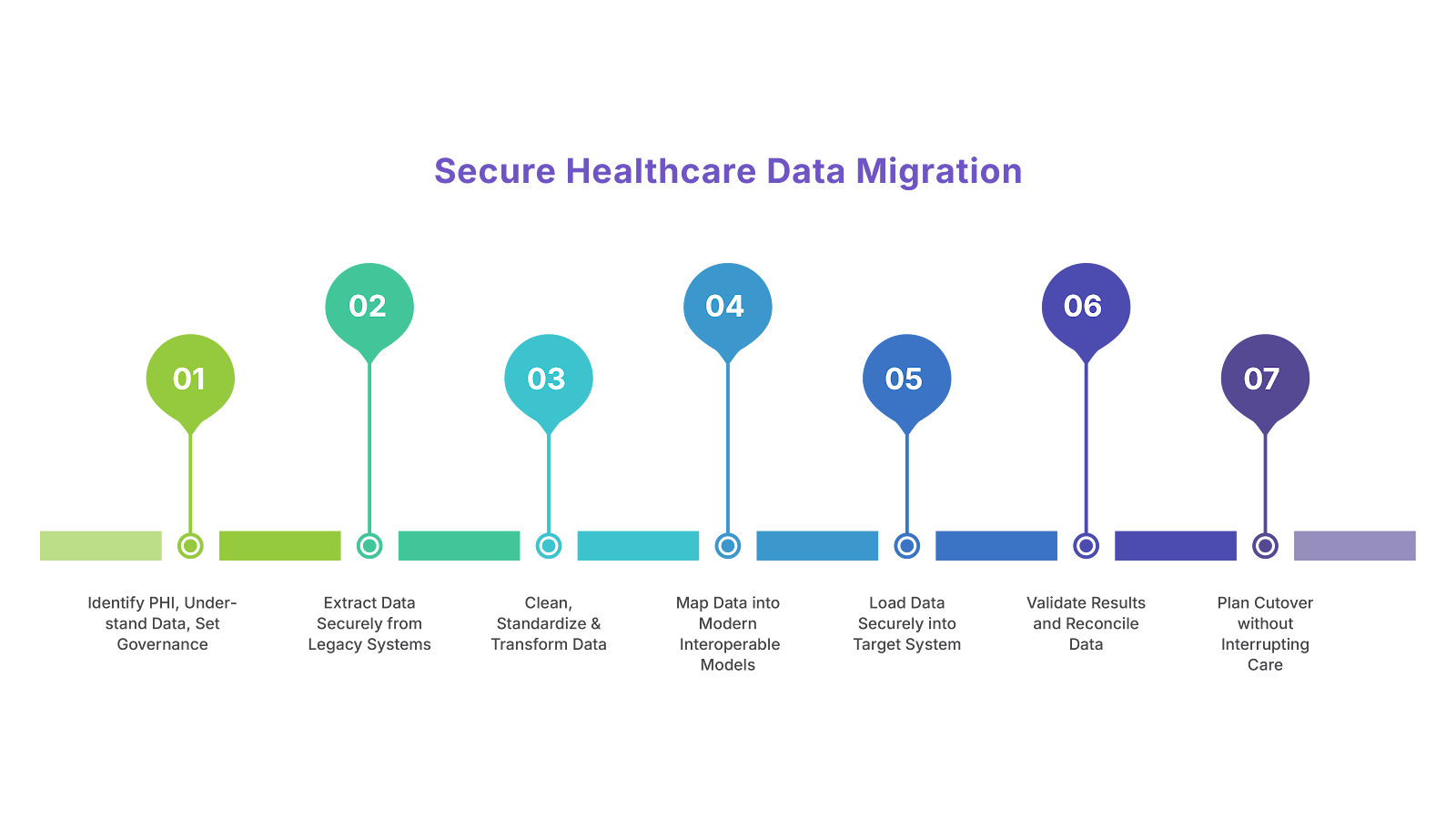
This is the step where teams slow down, look around, and map the digital terrain before touching anything.
It’s rarely just in the EHR. You’ll find PHI in lab interfaces, radiology dictations, scanned images, older departmental systems, and dark corners of legacy databases. Capturing this early prevents surprises later.
Some data — like diagnoses, meds, and vital signs — demands heightened protection. Other fields, like demographics or insurance metadata, still carry risk but require a different handling approach. Classification helps teams appropriately prioritize security controls.
Healthcare migrations fail when ownership is unclear. Data owners, clinical SMEs, stewards, and compliance leads must know precisely what they’re responsible for. When these roles are structured well, it reduces confusion and accelerates approvals.
dataZen catalogs data sources, identifies PHI, tags sensitive attributes, and establishes governance workflows to ensure organizations maintain complete visibility into their migration assets — all crucial for HIPAA compliance.
Extraction is often the riskiest phase because it is when PHI leaves its original, protected environment.
A secure pipeline is essential. Encryption ensures that even if something unexpected occurs — like a network issue — PHI remains unreadable to anyone without authorization.
Migration roles tend to expand quickly. A “least privilege” approach protects PHI by giving access only to those directly involved in the current task.
Every data pull should have a traceable record — who extracted it, when, how much, and from where. These logs protect the organization during audits and help pinpoint issues.
dataZap securely manages extraction, using encrypted pipelines and metadata-driven processes to ensure PHI never slips into logs or into exposed environments.
Once the data is out, the real work begins. Healthcare data is notorious for inconsistencies.
Duplicate records are common. A solid identity resolution process ensures each patient’s history remains intact and avoids misidentification downstream.
Mapping to ICD-10, SNOMED CT, CPT/HCPCS, and LOINC smooths interoperability and reduces friction when systems communicate.
Unusual lab values, inconsistent timestamps, or missing provider IDs might seem small, but they can quickly break workflows in a modern EHR. Addressing them now prevents trouble later.
dataZen enforces quality rules, and dataZense highlights anomalies through dashboards, making cleanup more collaborative and efficient.
This is where the heavy clinical intelligence comes in.
Every system organizes patients, encounters, allergies, meds, and labs differently. Mapping ensures data lands correctly — which affects everything from chart review to medication reconciliation.
FHIR resources like Patient, Observation, and Encounter follow a different logic than legacy HL7 segments. Getting this translation right affects interoperability and future readiness.
A visit type in one system may not exist in another. Medication structures may need remapping. Lab panels may break into individual results. This step blends clinical and technical thinking.
The mapping workbench provides versioning, transformation logic, and dependency tracking, ensuring mappings remain transparent and auditable.
Loading is not just about “inserting data into a new database.” It’s about ensuring relationships, sequence, and integrity remain intact.
Clinical data is interconnected. Encounters link to orders, labs, meds, imaging studies, and billing. If even one link breaks, the clinical picture becomes confusing.
Modern EHRs expect structured API interactions or validated batch files. Using these reduces risk and aligns with system expectations.
Even minor discrepancies — such as missing notes or mismatched timestamps — can frustrate clinicians. Load validation gives teams a chance to fix issues proactively.
dataZap handles API- and file-based loading with error detection, retries, and verification to maintain clinical integrity.
This stage is where teams confirm the migration didn’t just complete, but worked properly.
Record counts, field values, timestamps, and clinical descriptions must match. This prevents clinical risk and builds trust with frontline teams.
A physician knows if a medication list “looks right.” A pharmacist can detect an unusual order. Their insight often catches issues that automation alone misses.
Billing discrepancies can cause denials or compliance failures. Validating this early prevents revenue leaks.
dataZense provides reconciliation dashboards that highlight mismatches and help teams coordinate resolutions.
Good cutover planning is what separates a smooth go-live from a chaotic one.
Parallel operation helps teams identify mismatches in real time and ensures caregivers aren’t left scrambling during the switch.
New labs, admissions, vitals, and clinical notes continue to flow during the migration window. Incremental sync ensures nothing falls through the cracks.
This is a hub staffed with IT experts, clinicians, and vendor partners who monitor the transition and address issues quickly. It’s one of the most significant contributors to a calm go-live.
ChainSys SmartBots automate incremental syncs and ensure the legacy and target systems remain aligned.
Once the new system is live, the focus shifts to stability, compliance, and cleanup.
Role-based permissions and encryption settings must be verified immediately after go-live. This protects PHI from accidental exposure.
Early monitoring catches minor issues before they become disruptions. If clinicians report missing history or slow responses, the team can intervene quickly.
Keeping old systems running is expensive and risky. A compliant archival solution securely preserves PHI and enables organizations to decommission outdated platforms.
The archival solution stores historical data in a secure, searchable, read-only format — ideal for legal requirements, audits, and clinical lookup.
Best Practices for HIPAA-Compliant Healthcare Migration

Here are several practices that seasoned migration teams follow consistently:
Secure extraction, mapping, transformation, and loading — tailored to complex healthcare data models.
Governance, metadata, PHI identification, and business rule enforcement.
Data quality measurement, validation, and reconciliation dashboards.
Automation for real-time syncing, workflow triggers, and NZDT migrations.
Encrypted long-term storage for decommissioning legacy systems safely.
Healthcare migration is not just an IT project — it's a clinical responsibility. Every field, every timestamp, every data value carries meaning that clinicians rely on. The journey from legacy platforms to modern systems can feel overwhelming, but when handled with structure, clinical involvement, and strong governance, the outcome is transformative.
With a methodical, HIPAA-aligned approach and support from tools like the ChainSys Smart Data Platform, healthcare organizations can migrate safely, protect PHI, and prepare for a future where data is cleaner, more connected, and better able to support modern care.